“The more regularly you monitor your blood sugar levels, the more healthy lifestyle you lead.”
If you’re living with diabetes, here’s my first tip: Focus on the first part of the phrase. You are living! Diabetes will alter your life, yes, but your condition is something you are managing – not the other way around.
Travel is, for many people, a significant part of life. Whether you’re simply commuting to work or flying abroad to explore the most remote parts of the world, being able to get from A to B is essential.
Being mobile and independent allows us to do everything from solving the simplest problems to pursuing the greatest meaning. In other words, this is an important matter – almost as important as getting your meal plan right and having access to medicine and healthcare services.

Let’s start with the basics. When you travel – whether by air, sea or land – you expose your whole self to environments where the conditions for your wellbeing are unknown or unpredictable. In these situations, you will be less able to come to your own assistance when your body needs it.
But with a little preparation, you can anticipate most of the
challenges that are likely to come your way – and focus on the joy of
travelling instead of the risk. We will do a deeper dive into this in
the following sections.
Here is a tip which applies whether you are insulin dependent or
not: When you travel, make sure to check your glucose levels regularly
with a glucose meter – say, every 2 or 3 hours. Depending on the trend
of your glucose levels, your monitoring may tell you it is time for
injecting insulin or having a snack with fast-acting
carbohydrates.
“The more regularly you monitor your blood sugar levels, the more healthy lifestyle you lead.”
Getting used to checking your glucose levels regularly works sort of like an insurance policy! When you invest in taking full control, the payoff is increased freedom to make (and keep) plans, be spontaneous and have fun. It takes a little time and commitment, but it pays off.
Few things give people a stronger sense of freedom than getting behind the wheel of a car and taking off. You may need the car to commute to work in the morning, go out for groceries or get out of town for the weekend. Many people also operate a car or truck as part of their work.
Here is my tip: When you take your car – no matter where – pack with
forethought. Depending on what you keep your car stocked with, you can
turn your diabetic symptoms into little more than a blip in your
glucose levels, and avoid hypoglycaemia.
A little information about hypoglycaemia: Symptoms of hypoglycaemia tend to occur when glucose levels drop below 70 milligrams per deciliter of blood (3.9mmol/L). Common hypoglycaemic symptoms include:
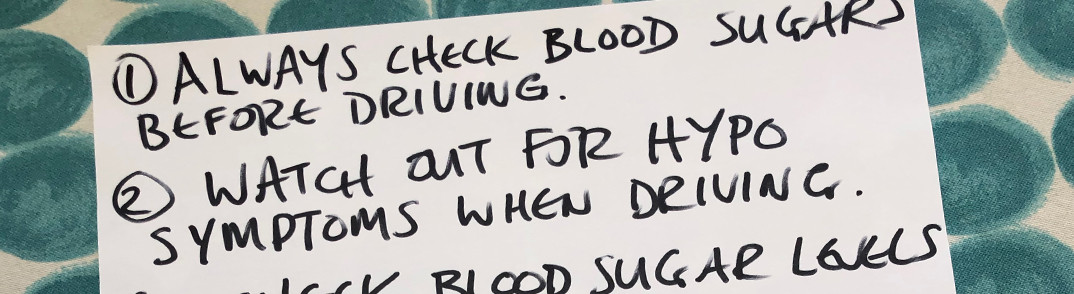
It goes without saying that you need to be completely in control of your body when you drive a car, so hypoglycaemia is something to avoid.

“Check your blood glucose levels before you get into the car. It’s not just something you should do. It’s something that legally you have to do.”
Before taking off, be sure to stock up on:
Here, “fast-acting carbs” refer to foods that cause a rapid increase
in your blood sugar levels. On the Glycaemic Index, which runs from 0
to 100, these foods occupy the 70-100 interval.
A couple extra tips: Check your blood glucose levels immediately before you get behind the wheel, and keep checking them every two hours during the course of your journey.
And lastly, reference the list above and pay attention to the symptoms you experience when your blood sugar levels drop. In the future, you’ll have increased awareness of how your body reacts, and you may be able to catch your glucose levels dropping at an earlier point in time.
Needless to say, if symptoms of hypoglycaemia occur while you’re
behind the wheel, pull over to a safe spot and don’t continue your
journey until your blood sugar is regulated.
Here’s another tip: The longer your journey and the farther away you go, the more you need to plan ahead. Write a checklist and include everything you might need in order to navigate every part of the journey. Regardless of your health, modern air travel can put stress on the body. This should be taken into consideration when you prepare for your trip.
“Prepare a check list for yourself. And bring enough medication to last you for your whole journey – and a little bit extra.”
Always board a flight with medication in your hand luggage – preferably a little more than you strictly need. If you are insulin dependent, ask your doctor beforehand to write a letter alerting the airline staff to your need to carry insulin, syringes and other supplies. Bring both your doctor’s letter and your prescriptions. Also, make sure that your pill bottles and insulin vials bear legible pharmacy labeling. These things will put you in a much stronger position if you are asked to explain your need to bring medical items onto a flight.
When you embark on a flight to a different time zone, log the time
and place you take your medication so as to not be thrown off by the
change in local time. Having your day either “shortened” or
“lengthened” by travel across time zones can destabilise your
metabolism. It is therefore your job to soften this impact and adapt
as precisely as possible to the new schedule and regimen. And logging
your time precisely is central to that end.
If possible, mention your trip to your doctor at least one month
before you leave. That way, he or she can help you plan for any
changes you may have to make to your insulin regimen.
Here are a few extra tips if you are insulin dependent. Keep your
insulin cool and pack it in an insulated bag to minimise the effect of
extreme changes in temperature. Refreezable ice gel packs or a frozen
or refrigerated bottle can also be used to keep your insulin cool.
Make sure to place a thin hand towel between the cooling device and
the medication so as to not expose your insulin directly to freezing
temperatures, as these will alter its effectiveness.
Note that being diagnosed with diabetes raises the risk of blood
clots, also called deep vein thrombosis (DVT). And whether diabetic or
not, flights of 4 hours or more have been associated with an increased
risk of DVT. To address that risk during a flight, I suggest that
you:
These tips may help lower the risk of DVT during air travel.

“Do as much research as possible in advance. Look at foods, look at medicines, look at sanitary conditions.”
Being diagnosed with diabetes does not mean you cannot travel the world. If you are visiting a culture where customs and attitudes deviate from your home culture, you may run into surprising and unforeseen reactions to your diabetes. The local population may, for example, think medical injections in public are an unusual and triggering occurrence. What has become routine and second nature to you may be a little shocking or disagreeable to another.
Besides being discrete and thoughtful towards your surroundings, do as much research ahead of time as possible:
Enjoy your trip and stay!

“Be as discrete and thoughtful as possible while injecting yourself, especially in a new culture where it can be seen as a little bit shocking and in-your-face.”
In principle, there is no activity you need to give up on completely when you’re diagnosed with diabetes. But it is crucial to develop a good sense of your own metabolic and emotional reactions to the things you either enjoy or have to do in your life.
If you are newly diagnosed, try to assume that you know nothing about yourself and have everything to learn. The less you take for granted about your body here and now, the more you will learn in the next minute – and the quicker you will adapt to living with diabetes.
This applies to travel-related activities, too. When you travel, you open yourself up to the world. In order to stay as safe as possible, you are required to take certain precautions. I suggest keeping a close watch on your blood sugar and general wellbeing. By planning ahead and learning from experience, you put yourself in the best possible position to take care of yourself and have a great time wherever you are.
Every diagnosis can lead to the worry that you will be unable to
pursue the things you love, the things that add meaning to your life.
I am here to tell you that while living with diabetes, you can still
tap into nearly all your favourite activities – you simply need to be
smart and careful about it. Start by taking the relevant precautions,
planning ahead, doing your homework and enjoying everything in
moderation.