Type 1 diabetes is a chronic autoimmune condition that affects individuals globally. While commonly diagnosed in children or young adults, it can develop at any age. However with daily management and the right support, people with type 1 diabetes can still lead full and active lives.1
Table of contents
What is type 1 diabetes?
Type 1 diabetes (T1D), also known as insulin-dependent diabetes, is an autoimmune disease in which your immune system mistakenly attacks insulin-producing beta cells in the pancreas. This leads to insulin deficiency. The lack of insulin secretion often requires insulin therapy for management1.
Type 1 differs from type 2 diabetes, which is commonly caused by insulin resistance more closely linked to lifestyle factors.1
Differences from other types of diabetes
It can be helpful to learn as much as you can about diabetes, starting with the main types:
- Type 1 diabetes: the autoimmune destruction of pancreatic beta cells, preventing your body from producing insulin1.
- Type 2 diabetes: primarily caused by insulin resistance, often associated with obesity and ageing1.
- Gestational diabetes: develops from pregnancy complications and typically resolves after birth, but increases the risk of type 2 diabetes later in life1.
We recommend you speak to your doctor if you have any specific questions about the differences between type 1 and type 2 diabetes.
The role of insulin
Insulin is critical in helping glucose enter your body’s cells for energy. In the absence of insulin, blood glucose builds up in the bloodstream, leading to very high blood sugar levels and other potential complications1.
Remember that type 1 diabetes is not caused by poor lifestyle choices. Type 1 diabetes has no known prevention and is influenced by genetic factors as well as environmental factors1.
Understanding life after a diabetes diagnosis
A type 1 diabetes diagnosis can feel life-altering. Many experience fear, anxiety, or grief as they come to terms with their symptoms. It's important to know that you're not alone and that there is help readily available to you for managing diabetes complications.
Educate yourself
Adjusting to life with type 1 diabetes involves learning new skills, including how to:
- Manage insulin
- Monitor your blood sugar levels
- Adjust the above in line with food intake and activity
Get the support you need
Research shows that education and early psychosocial support help to improve long-term outcomes of diabetes management1.
Type 1 diabetes symptoms
Early symptoms of type 1 diabetes can be easy to miss and may require a blood test for proper identification. Signs to look out for include9,10:
- Excessive urination: as your body expels excess glucose
- Extreme thirst: resulting from urination
- Muscle cramps: as fluid loss creates an imbalance in electrolytes in your blood
- Rapid weight loss: as your body uses fat for energy when cells cannot absorb glucose
- Tiredness and fatigue: as energy from glucose cannot reach your body’s cells
- Thrush/genital itching, yeast infections: as glucose in urine provides a breeding ground for fungus and bacteria
- Blurry vision: caused by high glucose levels in the fluid of your eye
- Sweet or fruity-smelling breath: as acids are released when your body uses non-glucose energy sources
Early diagnosis significantly improves health outcomes. If you or someone you know is experiencing any of these signs, it's important not to wait to get tested.
Different tests available
Tests your doctor may recommend include2:
- Random blood sugar test: to check your current blood sugar level
- Fasting blood sugar test: to assess blood sugar after a period of not eating
- Blood glucose meter: a handheld device that can measure your blood sugar level
- HbA1c test: gives an average of your blood sugar levels over the past 2–3 months
- Urine test: may detect glucose or ketones
- Autoantibody tests: to confirm type 1 diabetes, especially if the diagnosis isn’t clear
Diabetes-related complications
If type 1 diabetes is not diagnosed or managed early, it can lead to a range of short and long-term health complications. Delaying treatment can cause acute complications and increase the risk of developing more serious conditions over time, including1:
- Bacterial and fungal infections
- Cardiovascular disease
- Coronary artery disease
- Diabetic ketoacidosis (DKA)
- Diabetic retinopathy (damage to the retina)
- Digestive and kidney diseases
- Severe hyperglycemia or hypoglycemia from changes in blood glucose levels
- Very high blood pressure
Type 1 diabetes in everyday situations
Living with type 1 diabetes involves ongoing decisions and adjustments that can make a meaningful difference to your day-to-day life. Below are some general tips and advice for you to follow.
At school or work
- Communicate your needs with teachers or managers
- Keep fast-acting glucose and snacks on hand
- Plan for breaks to test blood sugar or insulin injections
Social life and eating out
- Use apps or carb guides to estimate meals
- Don’t be afraid to ask about ingredients
- Pre-bolus (inject insulin ahead of time) when needed
Travelling with type 1 diabetes
Structured preparation significantly reduces travel-related complications. Best practices for your travel plan include:
- Pack double the insulin, test strips, and supplies
- Keep insulin cool but avoid freezing
- Carry a medical ID and doctor’s letter
- Be aware of time zone changes for insulin timing
Talking to your doctor - what to ask
Whether you're newly diagnosed or have been living with type 1 diabetes for years, regular conversations with your doctor can make a big difference to your health and quality of life. Preparing questions ahead of time about next steps and treatment will ensure you cover what matters most to you.
Key questions to ask:
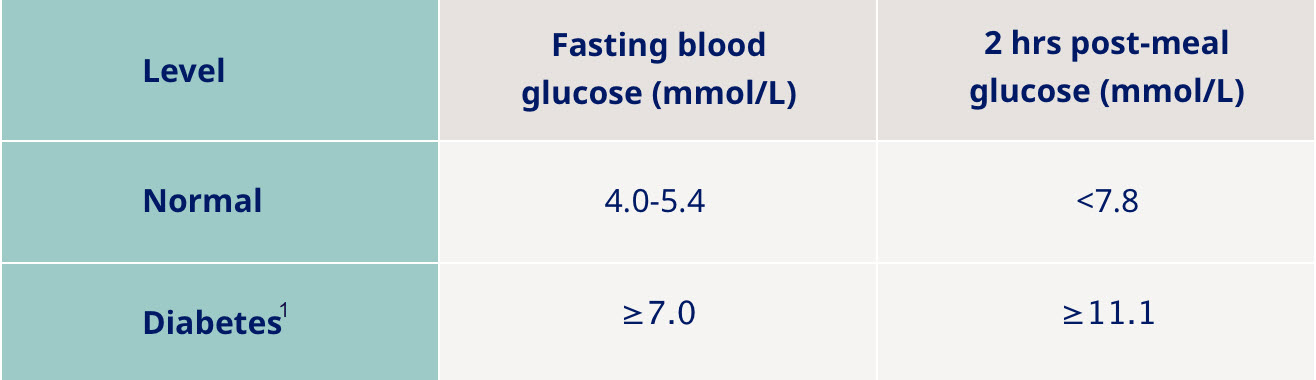
- What are my blood sugar targets?
Your ideal glucose range may depend on age, lifestyle, and health status. Clear targets help guide daily management and reduce risks of complications3.
- How do I adjust insulin for exercise, illness, or stress?
Physical activity and illness can cause unpredictable blood sugar changes. Understanding how to adjust your insulin can help prevent both highs and lows4.
- What complications should I be aware of?
Regular check-ups for eyes, kidneys, nerves, and heart health are vital. Ask which screenings you need and how often1.
- Is a CGM or insulin pump right for me?
Technologies like continuous glucose monitors (CGMs) and insulin pumps can improve control and reduce the burden of diabetes management. Your doctor can help you explore what’s best for your lifestyle5.
Real stories and real strength
Living with diabetes is different for everyone. But hearing real stories from adults, parents and young children can provide comfort and remind you that while your condition presents challenges, it doesn’t define who you are. Advancements in diabetes technology mean you can also live normally in many aspects of your life.
The power of community support
The support you receive and give can also help reduce feelings of isolation, build confidence in managing your daily care, and remind you that you don’t have to live alone with your diagnosis.
With the right knowledge, tools, and support, living with type 1 diabetes therefore becomes far less of a burden and something that can be effectively managed as part of your everyday life.
FAQs
I’ve just been diagnosed. What should I do first?
First, take a breath - you’re not expected to know everything right away. Start by speaking openly with your doctor or healthcare professional and asking for practical guidance. Consider finding support through communities or groups that can help you take one step at a time.
Will I ever be able to travel or eat normally again?
Yes, you can absolutely travel, eat out, and enjoy life. It may take a bit more planning than before to maintain average blood sugar levels , but with the right tools and preparation, you can adapt. Many people with type 1 diabetes go on adventures, try new foods, and live globally.
Are there others going through the same thing?
Definitely, millions of people live with type 1 diabetes, and many share similar questions and concerns. Support groups, online forums, and patient communities can be a great way to connect, share tips, and feel understood.
ZA25DI00097 October 2025
References
- International Diabetes Federation. IDF Atlas 10th Edition, 2021. Available from: https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF Atlas 10th Edition 2021.pdf. Last accessed: May 2022.
- American Diabetes Association. Classification and Diagnosis of Diabetes. Diabetes Care. Available at: https://diabetesjournals.org/care/article/46/Supplement_1/S19/148056/2-Classification-and-Diagnosis-of-Diabetes. Last accessed May 2025.
- American Diabetes Association. Standards of Medical Care in Diabetes—2024. Diabetes Care. 2024;47(Suppl 1):S1–S350.
- Riddell MC, Gallen IW, Smart CE, et al. Exercise management in type 1 diabetes. Lancet Diabetes Endocrinol. 2017;5(5):377–390.
- Foster NC, Beck RW, Miller KM, et al. State of Type 1 Diabetes Management and Outcomes from the T1D Exchange. Diabetes Technol Ther. 2019;21(2):66–72.

