Type 1 diabetes treatments
Understanding the types of type 1 diabetes treatments available and how they get close to your body’s natural insulin response.
Meet Quinn who shares her experience on living with type 1 diabetes
Type 1 diabetes (T1D), also known as insulin-dependent diabetes, is an autoimmune disease in which your immune system mistakenly attacks insulin-producing beta cells in the pancreas. This leads to insulin deficiency. The lack of insulin secretion often requires insulin therapy for management1.
Type 1 differs from type 2 diabetes, which is commonly caused by insulin resistance more closely linked to lifestyle factors.
It can be helpful to learn as much as you can about diabetes, starting with the main types:
We recommend you speak to your doctor if you have any specific questions about the differences between type 1 and type 2 diabetes.
Insulin is critical in helping glucose enter your body’s cells for energy. In the absence of insulin, blood glucose builds up in the bloodstream, leading to very high blood sugar levels and other potential complications5.
Remember that type 1 diabetes is not caused by poor lifestyle choices. Type 1 diabetes has no known prevention and is influenced by genetic factors as well as environmental factors6.
A type 1 diabetes diagnosis can feel life-altering. Many experience fear, anxiety, or grief as they come to terms with their symptoms. It's important to know that you're not alone and that there is help readily available to you for managing diabetes complications.
Adjusting to life with type 1 diabetes involves learning new skills, including how to:
Research shows that education and early psychosocial support help to improve long-term outcomes of diabetes management7.
General social and emotional support also plays a powerful role. Peer groups and counselling services can significantly help reduce diabetes-related distress8.
Early symptoms of type 1 diabetes can be easy to miss and may require a blood test for proper identification. Signs to look out for include9,10:
Early diagnosis significantly improves health outcomes. If you or someone you know is experiencing any of these signs, it's important not to wait to get tested.
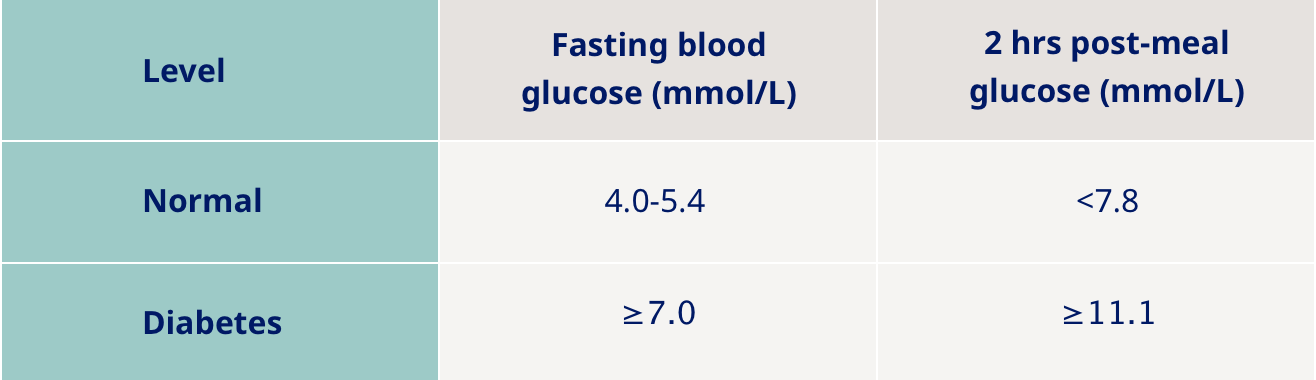
Tests your doctor may recommend include11:
If type 1 diabetes is not diagnosed or managed early, it can lead to a range of short and long-term health complications. Delaying treatment can cause acute complications and increase the risk of developing more serious conditions over time, including:
Living with type 1 diabetes involves ongoing decisions and adjustments that can make a meaningful difference to your day-to-day life. Below are some general tips and advice for you to follow.
Studies confirm that structured preparation significantly reduces travel-related complications. Best practices for your travel plan include12:
Whether you're newly diagnosed or have been living with type 1 diabetes for years, regular conversations with your doctor can make a big difference to your health and quality of life. Preparing questions ahead of time about next steps and treatment will ensure you cover what matters most to you.
Living with diabetes is different for everyone. But hearing real stories from adults, parents and young children can provide comfort and remind you that while your condition presents challenges, it doesn’t define who you are. Advancements in diabetes technology mean you can also live normally in many aspects of your life.
Whether in-person or online, community support from the diabetes community can be a powerful tool in diabetes care that you can benefit from and contribute to. In fact, research shows that people who engage in peer support often feel more empowered and better equipped to manage their diabetes day-to-day17.
The support you receive and give can also help reduce feelings of isolation, build confidence in managing your daily care, and remind you that you don’t have to live alone with your diagnosis.
With the right knowledge, tools, and support, living with type 1 diabetes therefore becomes far less of a burden and something that can be effectively managed as part of your everyday life.
First, take a breath - you’re not expected to know everything right away. Start by speaking openly with your doctor or healthcare professional and asking for practical guidance. Consider finding support through communities or groups that can help you take one step at a time.
Yes, you can absolutely travel, eat out, and enjoy life. It may take a bit more planning than before to maintain average blood sugar levels , but with the right tools and preparation, you can adapt. Many people with type 1 diabetes go on adventures, try new foods, and live globally.
Definitely, millions of people live with type 1 diabetes, and many share similar questions and concerns. Support groups, online forums, and patient communities can be a great way to connect, share tips, and feel understood.
HQ25DI00124