
Diabetes in children
Learn more about diabetes in children and the support they may need to help manage their condition.
What are the differences between type 1 and type 2 diabetes? Discover what’s happening in your body, symptoms and how to manage the disease.
There are three main types of diabetes – type 1, type 2 and gestational. It is estimated that 537 million people have diabetes worldwide. Type 2 diabetes is by far the most common, accounting for over 90% of those cases1.
Gestational diabetes is when you develop high blood sugar during pregnancy, which can happen because of hormone changes that occur in your body during this time1.
Learn more on gestational diabetes here. There is also a form of diabetes called latent autoimmune diabetes in adults (LADA). The symptoms are similar to type 1 and type 2, but LADA generally presents a bit later on and symptoms develop slower than in type 1 diabetes, but faster than type 2 diabetes. People with LADA also tend to be a healthy weight. LADA, sometimes called type 1.5 diabetes, is not classified as a separate type of diabetes, falling somewhere between type 1 and type 2. If you have LADA you will usually start taking a form of oral medication called metformin, and move onto insulin as your blood sugar levels start to go up. Research into LADA is ongoing and there currently isn’t a definite, agreed way of managing the condition2.
You can develop type 1 diabetes at any age, although it tends to be more common in children and young adults. It occurs when your immune system attacks itself and destroys cells in your pancreas that make insulin. As a result, your body can’t make insulin, or makes very little, and without insulin your body can’t process blood sugar. Instead of being absorbed into your cells and used as energy, this blood sugar builds up in your bloodstream, damaging the body and leading to diabetes symptoms and complications1. Diet and lifestyle habits do not cause type 1 diabetes3. Familial genetics can play a role in the development of this condition in some cases, but this is not fully understood4.
Type 1 vs Type 2 diabetes - Type 2 diabetes differs from type 1 diabetes in that you do produce insulin, but your body does not use it properly – this is called insulin resistance. As a result, your body needs more insulin to help absorb blood glucose into your cells. At first, your pancreas makes more insulin to compensate for this, but over time the pancreas can’t make enough insulin and your blood glucose levels rise. Lifestyle factors such as lack of exercise or having overweight can be a factor in the development of type 2 diabetes5.
Experts still do not know exactly what causes type 1 diabetes; however, the following are thought to be linked:
There are several factors that can increase your risk of developing type 2 diabetes, including7:
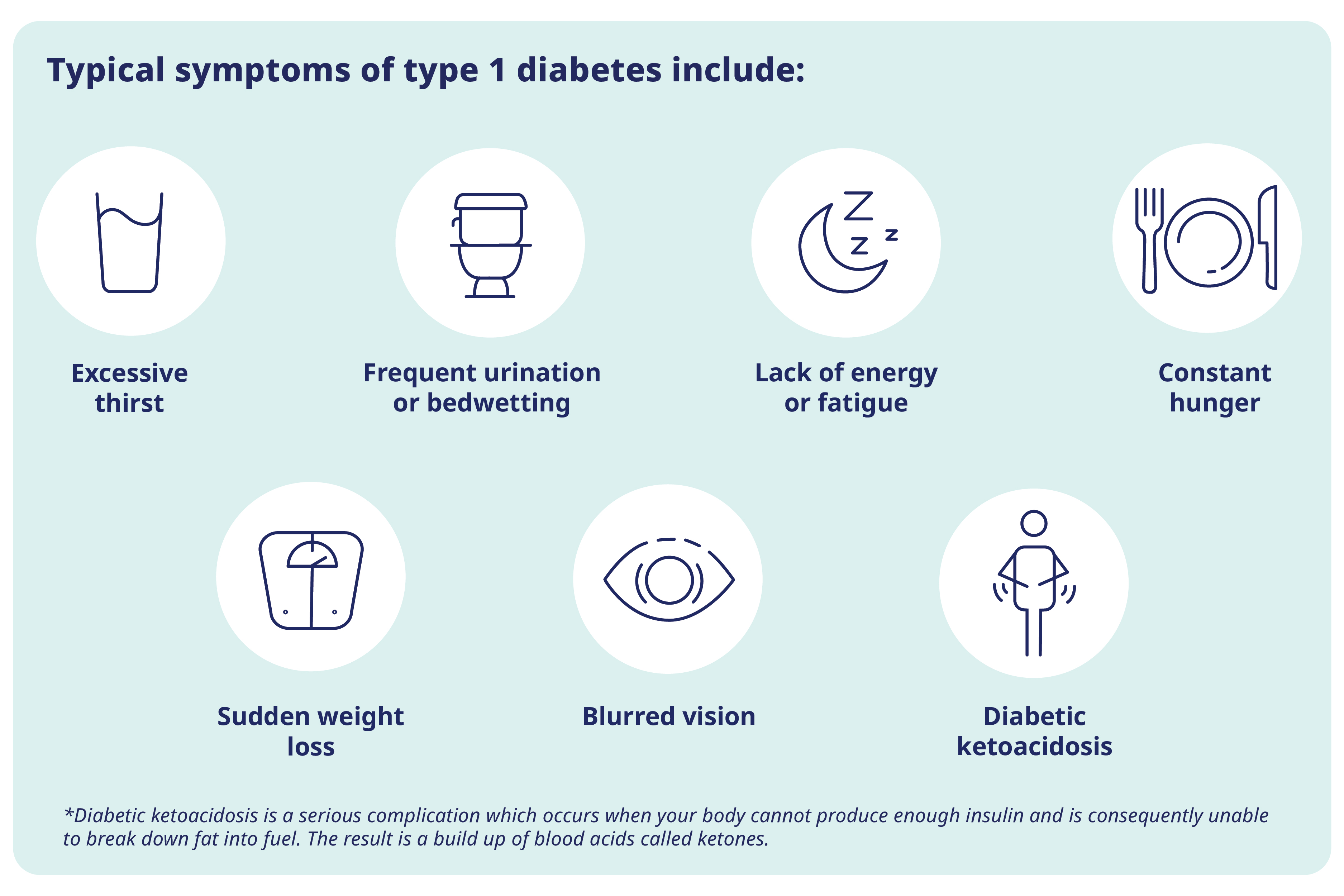
Symptoms in type 2 diabetes can be the same as above1, but could also include:
Diabetes symptoms can be similar for both type 1 and type 2, but in general, symptoms for type 2 diabetes can be a lot less noticeable, or you may not experience any, which can result in a delayed or missed diagnosis1. While symptoms for type 1 diabetes tend to appear quickly, those for type 2 diabetes can appear more slowly, which can also lead to them being missed6.
Find out more about diabetes symptoms here.
People living with type 1 diabetes require daily insulin injections to manage their condition. In contrast, treatment options for type 2 diabetes focus on lifestyle changes; if these are not enough to manage blood glucose levels, medication may also be required1.
As people living with type 1 diabetes make little to no insulin, daily insulin injections are required to help manage blood glucose levels. You can live a healthy life, and delay or prevent diabetes-related complications if you monitor your blood glucose, visit a healthcare professional regularly, and get support from family and/or loved ones1,3. To find out more about treatment for type 1 diabetes, read our article here.
A key part of treating type 2 diabetes is trying to lead a healthy lifestyle, which may include following a healthy and balanced diet, taking part in regular physical activity, avoiding smoking and trying to maintain a healthy body weight1.
Most people with type 2 diabetes do not require insulin therapy but, if lifestyle changes aren’t enough, they may require medications such as metformin, glucagon-like peptide-1 receptor agonists (GLP-1 RAs), dipeptidyl peptidase-4 inhibitors (DDP-4is), sodium-glucose cotransporter-2 inhibitors (SGLT-2is) or insulin1.
To find out more about treatment of type 2 diabetes, read our article here.
One-third to half of people with type 2 diabetes may be undiagnosed1.
January 2024. IE23DI00189