WHAT IS DIABETES?
Understanding diabetes - a simple overview
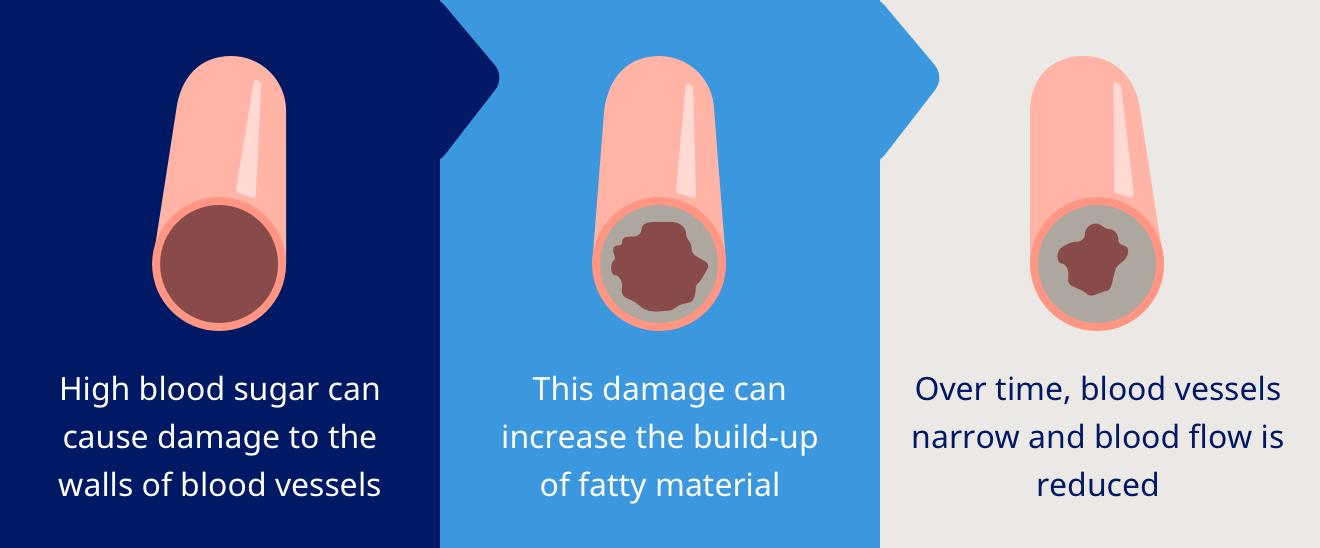
Diabetes mellitus, commonly referred to as diabetes, is a chronic disease that affects how the body turns food into energy. It is not the result of personal failure, poor lifestyle choices, or a lack of willpower. Instead, diabetes develops due to a mix of genetic, environmental, and lifestyle factors that impact insulin production and blood sugar regulation1.