What is type 1 diabetes?
Understanding the difference between type 1 and type 2 diabetes and recognizing the common symptoms of type 1 diabetes.

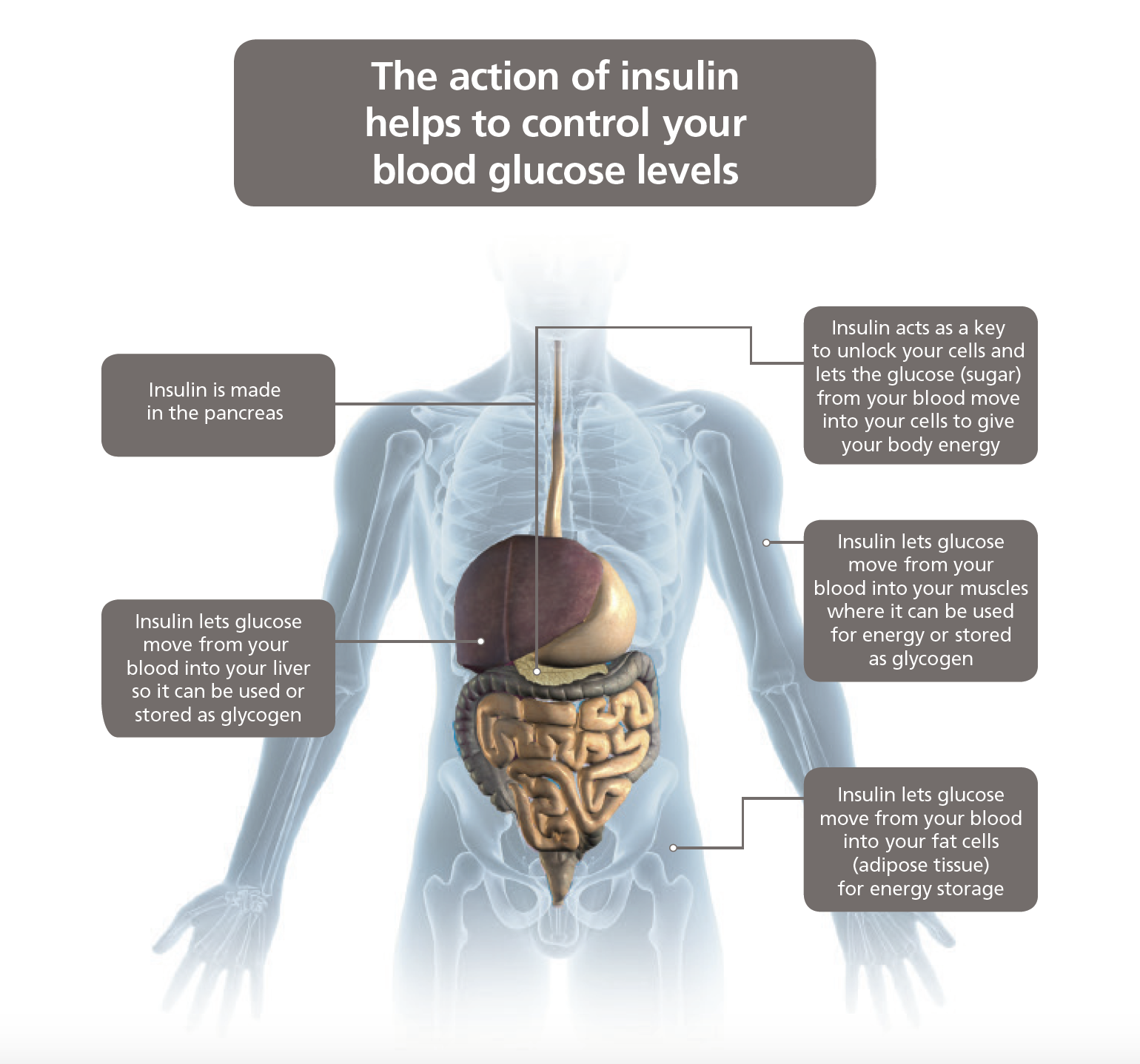
Type 1 diabetes is an autoimmune disorder. In type 1 diabetes the insulin-making cells in the pancreas known as ‘islet’ or ‘beta’ cells are destroyed. There are certain genetic factors which make some individuals more vulnerable to developing type 1 diabetes. Factors in the environment also contribute and research is ongoing to try to understand these better. Type 1 diabetes starts more frequently in young people and insulin is always needed from diagnosis.
Insulin is the most common treatment for type 1 diabetes. Without it, people with type 1 diabetes wouldn’t survive. Insulin treatment aims to get as close as possible to the natural insulin response of someone without diabetes. This can help people with type 1 diabetes keep insulin levels balanced and maintain healthy blood glucose (sugar) levels, which is important to avoid damage to health later in life.
People with type 1 diabetes need daily injections of insulin to survive. Insulin treatment aims to get as close as possible to the natural insulin response of someone without diabetes. This can help people with type 1 diabetes keep a balance of the right amount of insulin to maintain balanced blood glucose levels, which is important to stay healthy and avoid damage to health later in life.
There are several types of insulin treatments available for type 1 diabetes. Speak to your doctor to discuss available treatment options to tailor your diabetes treatment to your specific needs and preferences.
Provides a constant, steady release of insulin throughout the day (intermediate or long acting).
Brings down spikes in blood glucose (sugar) after eating
Combines two insulins in a single injection
Basal insulin treatment aims to match the constant, steady release of insulin in someone without diabetes. It keeps a low, consistent insulin level in your blood over an extended time to keep your blood glucose levels steady throughout the day, including between meals and when you sleep.
Basal insulin must get close to a natural insulin response. Too much or too little insulin can cause hypoglycaemia (low blood glucose (sugar)) or hyperglycaemia (high blood glucose (sugar)) respectively.
Your blood sugar rises rapidly after eating, and sometimes, basal insulin treatment isn't enough to control these 'spikes'. Mealtime insulin (also called bolus insulin) treatment aims to bring down such spikes in blood glucose (sugar) that can occur after eating. The closer that mealtime insulin treatment can get to the insulin response in someone without diabetes, the quicker it may be able to bring down these spikes.
There are different types of insulin available for managing mealtime spikes. The latest generation of ultra-fast acting mealtime insulins aims to close the gap between the speed of insulin treatment and the natural insulin response. As a result, they may improve control of mealtime blood glucose (sugar) and offer greater flexibility and convenience with insulin dosing, mealtimes, and food choices. These benefits may reduce some of the guesswork in pre-meal dosing and provide greater blood glucose control for people with type 1 diabetes.
Another type of insulin treatment is premixed insulins. Premixed insulins combine two insulins in a single injection and aim to replicate the insulin production in the body of someone without diabetes when fasting (between meals and overnight) and after a meal.
Insulin needs to be taken by injection beneath the skin or by infusion with an insulin pump. Unlike GLP-1 RAs, insulin cannot be given as a tablet because the digestive system would break down the insulin in the stomach before it could start working.
Many people take insulin by injection. A wide range of pens and needles are available for insulin injections depending on your requirements. These have been designed to be ultra-discreet and easy to use.
They can be pre-filled and disposable or refillable and durable. Some have a memory function and/or require only minimal pressure to operate them, making them suitable for many users, including children as young as six years old and the elderly population.
Some people with type 1 diabetes take their insulin using a small, computerised insulin pump device. Insulin pumps provide the body with insulin throughout the day. The idea is that instead of delivering separate injections during the day, an insulin pump releases insulin gradually over the day, just like your body would naturally.
An insulin pump is essentially made up of two parts (which are connected by a small, flexible tube):
![]()
The insulin pump is fitted onto a person’s lower abdomen, held in place with an adhesive patch, or worn in a belt around the waist, armband, bra, or other accessories. The average pump is about the size of a pack of cards and has a digital display screen and buttons for programming.
There are lots of different types of insulin pumps available with different features. For example, some more modern pumps have touchscreens or can connect wirelessly to a glucometer. Your doctor will be able to help you select a model that’s best suited to your needs and lifestyle.
Information placed on this webpage is not intended as a substitute for consultation with your healthcare professional
January 2024. IE23DI00249