Frequently asked questions about treatment of diabetes
Find some of the common questions and concerns about starting diabetes treatment.

Diabetes treatment options for type 2 diabetes typically focus on lifestyle changes such as healthy eating, regular exercise, and weight loss. Most people with type 2 diabetes do not require insulin therapy but may require other medications, for example metformin, glucagon-like peptide-1 receptor agonists (GLP-1 RAs), dipeptidyl peptidase-4 inhibitors (DDP-4is) or sodium-glucose cotransporter-2 inhibitors (SGLT-2is) as the disease progresses. 2
In comparison, type 1 diabetes is harder to control, and treatment options are a little more complex. People who have type 1 diabetes must follow a strict regimen of daily insulin injections. 2
Diabetes occurs when your body cannot produce any insulin (Type 1) or enough insulin to cover what your body needs (Type 2). Explore diabetes treatment options in this section - including medications, diet and exercise plans.
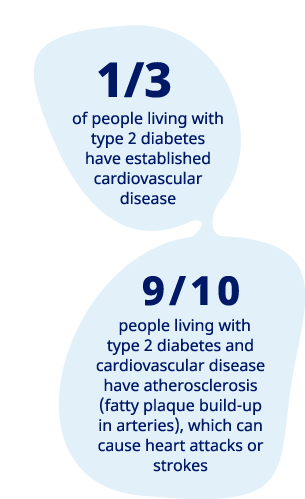
People with type 2 diabetes are 2-4 times more likely to have a heart attack or stroke compared to someone living without diabetes. 3,19
Learn how you can reduce the risk.
People with type 1 diabetes are unable to produce enough insulin to regulate blood glucose levels due to their immune system attacking their pancreas. People with type 1 diabetes need daily insulin injections (mimicking the natural response of the pancreas). 2
Long-acting insulin that provides a constant and steady release of insulin. Basal insulin keeps a low and consistent level of insulin in your blood over a period of time and is usually administrated once or twice daily.
Fast-acting insulin that brings down spikes in blood sugar after eating. Mealtime insulin is injected before you eat and is sometimes taken in addition to long-acting insulin.
Combines two insulins in a single injection. Premix insulins help control blood sugar throughout the day (copying the role of basal insulin) and during mealtimes (copying the role of mealtime insulin). Note, premix insulins are more often prescribed to people with type 2 diabetes.
Injections
Insulin pens are one of the most common ways to self-administer insulin daily. Many pens are available, including pre-filled disposable pens and refillable durable pens. 6
Insulin pumps
A small, computerised device, known as an insulin pump, can be used to administer insulin for people with type 1 diabetes. An insulin pump works by gradually releasing insulin over the course of the day. 6
Insulin has long been an essential treatment of type 1 diabetes, but are there alternative treatment methods available as science and medicine progress?
Pancreatic islet transplantation is one experimental treatment for type 1 diabetes, currently undergoing clinical trials in the US. Doctors take islets (from the pancreas) with healthy beta cells and inject them into a vein that carries blood to the liver. The islets begin to make and release insulin inside the recipient’s body. A phase 3 clinical trial conducted by the National Institutes of Health (NIH) found that '1 year after islet transplantation, nearly 9 out of 10 transplant recipients had an A1C level below 7 percent and did not have episodes of severe hypoglycemia' . 7
Once-weekly insulin is another promising research area for treatment of both type 1 and type 2 diabetes. Some companies are looking into developing basal insulin that can be administered once a week, which would make it easier for most to follow treatment plans. In 2021, findings from a trial with type 2 diabetes participants were published with promising results. 14,15
Research into alternative treatment of type 1 diabetes continues, but stem cell-based implants seem to be at the forefront of testing. Natural treatment for diabetes and permanent treatment for diabetes are also progressive research areas.
Type 2 diabetes treatment guidelines are considerably different to type 1 treatment guidelines. While type 1 is dependent on insulin injections, type 2 diabetes can be treated initially without medication, but may require other medications, for example metformin, GLP-1 RAs, DDP-4is or SGLT-2s as the disease progresses. 2
Changing your diet is the first thing you’ll be asked to do when diagnosed with type 2 diabetes. Diabetes diet plans are designed to keep blood glucose, blood pressure and cholesterol at healthy levels.
An increase in physical activity each day can also make a real difference to your health. Regular diabetes exercise helps control your blood sugar level, lose weight and improve your physical and mental health.
GLP-1 is a naturally occurring hormone that increases incretin hormones and helps to produce insulin, thus reducing glucose in the blood. GLP-1 RA treatments aim to mimic the natural function of the GLP-1 hormone and balance your blood glucose levels. There are different types of GLP-1 RAs:
Sodium-glucose cotransporters-2 inhibitors (SLGT-2is) are an oral medication used to lower blood glucose levels by causing the kidneys to remove sugar from the body through urine.
If a combination of the above treatment methods isn’t working or has stopped working, you may move on to insulin injections. Remember, there are different types of insulin, and they vary depending on how quickly they work, when they have the greatest effect and how long they work.
Remember, type 2 diabetes is a progressive disease and often a diabetes treatment algorithm is used as a tool to determine treatment. Don’t be disheartened if your treatment plan changes over time. 11
Gestational diabetes treatment
Simply changing your diet and exercise routine is enough to combat gestational diabetes for some pregnant women. For others, medication and insulin injections are required to balance blood sugar levels. 2 Metformin and glibenclamide tablets are frequently given to pregnant women; speak with your healthcare professional if you have concerns. 12,13
Child diabetes type 1 treatment
To keep your child’s blood glucose at healthy levels, they’ll need daily insulin injections. Blood glucose monitoring, carbohydrate counting and regular exercise are also strongly recommended. 2
Child diabetes type 2 treatment
Type 2 diabetes in children is similar to pre-diabetes symptoms and treatment in adults. Healthy eating, regular exercise, blood glucose monitoring and weight loss will all help stay on top of your child’s diabetes. In some instances, medication will need to be administered. 2
January 2024. IE23DI00246