Atherosclerosis is the main cause of cardiovascular disease (CVD), and atherosclerotic cardiovascular disease (ASCVD) is particularly common in people living with type 2 diabetes. Nine out of ten people with type 2 diabetes and established cardiovascular disease have atherosclerotic cardiovascular disease, including heart attack and stroke.
Your doctor or diabetes specialist nurse may already have discussed the connection between type 2 diabetes and heart disease with you and you may already be taking steps to reduce your risk. However, many people with type 2 diabetes are unaware that they have increased risk of developing cardiovascular disease. If you have type 2 diabetes, you have about twice as much risk of having cardiovascular disease as people without diabetes. In fact, one-third of people living with type 2 diabetes have established cardiovascular disease.
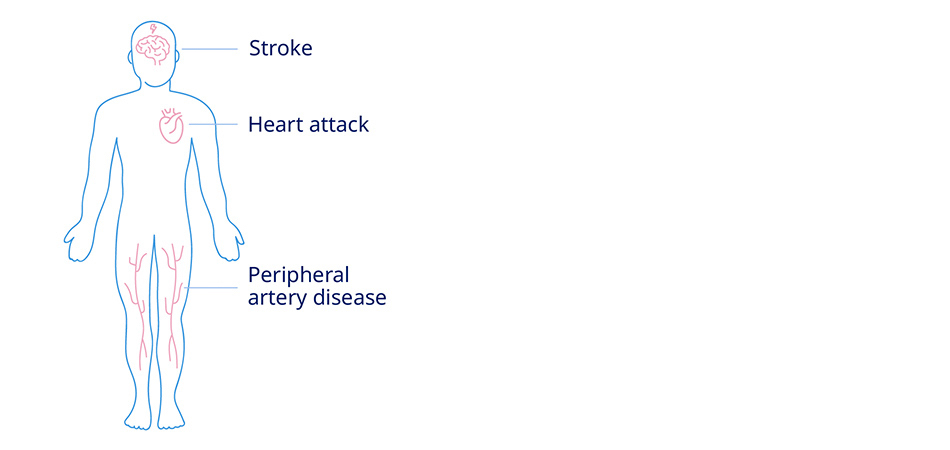
Cardiovascular disease is a general term for a wide range of conditions affecting your heart or blood vessels and includes, but is not limited to, high blood pressure, heart failure, peripheral artery disease (PAD), angina (chest pain caused by reduced blood flow to the heart muscles), heart attacks and strokes.
Atherosclerosis is the main cause of cardiovascular disease, and atherosclerotic cardiovascular disease (explained further below) is particularly common in people living with type 2 diabetes because excess blood sugar fuels the progression of atherosclerotic cardiovascular disease. Nine out of 10 people with type 2 diabetes and cardiovascular disease have atherosclerotic cardiovascular disease.
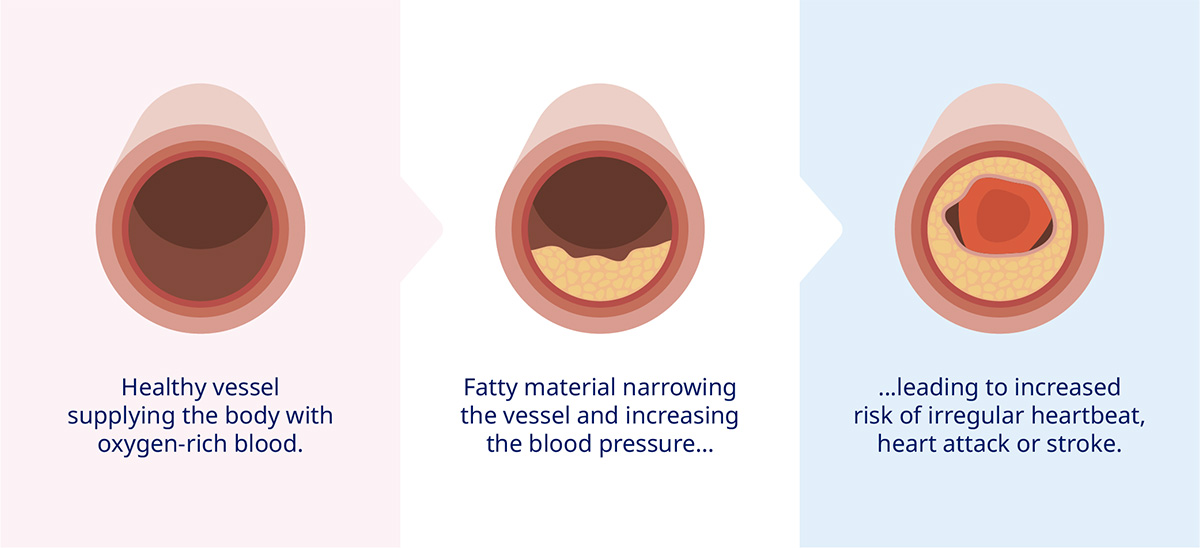
Atherosclerosis is the build-up of fats, cholesterol and other substances in your arteries and on your artery walls. This build up is called plaque. The plaques cause your arteries to harden and narrow, restricting blood flow and oxygen supply to your organs. Potentially the plaques can also burst, leading to a blood clot. If the blood flow to your heart is blocked it can cause a heart attack and if a blood clot blocks an artery in your brain, this causes a stroke.
Atherosclerosis can also cause problems in other parts of your body. Peripheral artery disease, for example, is caused when blood flow is restricted in the arteries in your legs. Peripheral artery disease can cause pain in your calves, hips, buttocks and thighs – usually when you’re walking or exercising.
Atherosclerosis develops over years and does not tend to have any symptoms at first. Thus, many people may be unaware that they have it. Sometimes people only find out they have atherosclerotic cardiovascular disease when they have a stroke, transient ischaemic attack (TIA, or mini-stroke) or heart attack.
How atherosclerotic cardiovascular disease can lead to the formation of plaques
Doctors used to believe that high cholesterol was the driving force behind the formation of atherosclerotic plaques and that reducing cholesterol levels through lifestyle and medication was the key to managing the condition. However, we now know that high blood sugar is an important factor. High blood sugar results in inflammation, causing damage to the arterial wall and causes plaques to form. This supports why people with type 2 diabetes are 2–4 times more likely to have a heart attack or stroke than those without the condition.
There are other factors that contribute to atherosclerotic cardiovascular disease risk such as overweight and obesity, smoking and high blood pressure. Together with high blood sugar, these are all called ‘modifiable’ risk factors because it is possible to reduce the impact of these factors with lifestyle changes and medications.
The good news is that there are many ways to reduce the risks of atherosclerotic cardiovascular disease events and many of these will not only improve your general health but also help prevent consequences of your diabetes too. Here are some lifestyle changes that you can make.