
How to lower your heart disease risk
Managing your type 2 diabetes can also lower your risk of heart disease. Learn what you can do for both.
Meet Lynn Berriger who was hit by a heart attack
Are cardiovascular disease and heart disease the same thing? In short, no - cardiovascular disease is an umbrella term for conditions that affect the heart (cardio) or blood vessels (vascular) and covers all heart and circulatory diseases3, including:
Heart disease is another broad term used to describe a range of disorders affecting your heart, and these include4:
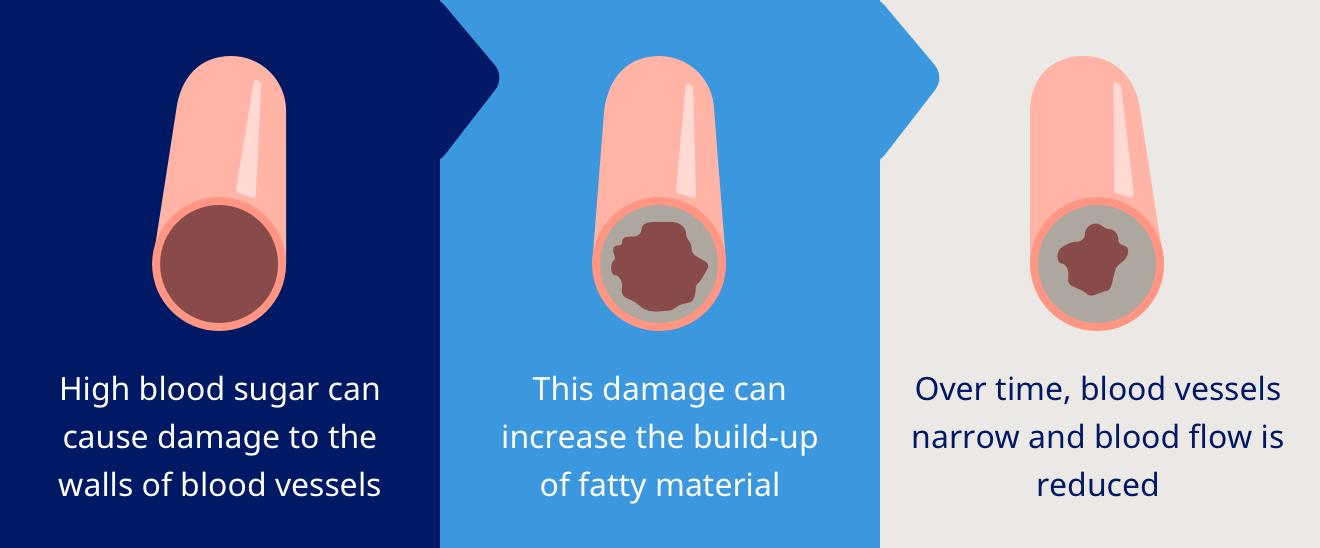
There’s a strong correlation between both cardiovascular disease and diabetes and heart disease and diabetes1,2,5. In both, blood vessels narrow and the amount of oxygen-rich blood reaching the body’s vital organs is severely reduced5.
The blood pressure rises, and your heart must work harder to move blood around the body. Over time, this can cause lasting damage to the heart, resulting in cardiovascular disease5.
Both type 1 and type 2 diabetes have established risk factors for cardiovascular disease6.
You’ll likely already be familiar with the symptoms of type 2 diabetes, and this knowledge will come in handy when exploring the correlation between type 2 diabetes and cardiovascular disease.
As a quick refresher, note that type 2 diabetes causes high glucose levels in the bloodstream7. This can quickly lead to the damaging of blood vessel walls, an increase in fatty materials and the reduction of blood flow. This kind of build-up can starve the heart of oxygen and nutrition, potentially resulting in severe heart conditions, strokes, and high blood pressure5,8.
Symptoms of cardiovascular heart disease to look out for as a patient with type 2 diabetes can include9:
Uncontrolled blood sugar levels in people with diabetes damage the walls of the blood vessels, speeding up a process called atherosclerosis, which can lead to strokes. People with diabetes also tend to have high levels of the types of fats in their blood that get turned into plaques, another contributor to strokes8. Diabetes stroke symptoms include10:
Although post-stroke patients with diabetes are predisposed to a slower recovery of function, diabetes stroke recovery is possible11. A successful recovery requires the brain to remap sensorimotor functions within the brain network12.
When it comes to managing cardiovascular disease, preventative efforts are key13. Patients with type 2 diabetes should turn to medication, lifestyle changes and risk factor interventions to reduce their risk of cardiovascular disease14. Note, every condition is different and reducing the risk of cardiovascular disease will require a different approach from person to person.
If you have any type of diabetes (type 1, type 2, gestational, adolescent) you should pay close attention to your lifestyle habits. Lifestyle factors that promote narrowing or clogging of blood vessels, and increase the risk of cardiovascular disease, include:
Clinical evidence shows that a cholesterol level reduction may lower the mortality rate from cardiovascular disease15.
A nutritionally limited or poor diet can lead to high blood pressure. Try to reduce your daily sodium intake16.
Smoking is a significant risk factor for strokes17. Tobacco is known to damage and narrow blood vessels17.
There is also a positive correlation between the reduction of body fat and insulin sensitivity. Addressing weight loss (physical activity is one of many options) is key to achieving steady blood sugar levels18.
Exercising more, eating a balanced diet to lose weight, and cutting out bad habits like excessive drinking and smoking are all great ways to reduce your risk of cardiovascular disease15-18.
While lifestyle changes are important for reducing the risk of cardiovascular disease, it’s also imperative that you continue to monitor blood sugar level carefully and manage your medication13,14.
HQ25DI00011

