
How to lower your heart disease risk
Managing your type 2 diabetes can also lower your risk of heart disease. Learn what you can do for both.
Lynn Berriger's story on recovering from a heart attack
Cardiovascular disease (CVD) remains the leading cause of death globally, including conditions like coronary heart disease and is responsible for an estimated 17.9 million deaths per year - approximately 32% of all global deaths1. In people with type 2 diabetes, the risk of developing cardiovascular disease is significantly higher due to the long-term impact of elevated blood glucose on the arteries and heart.
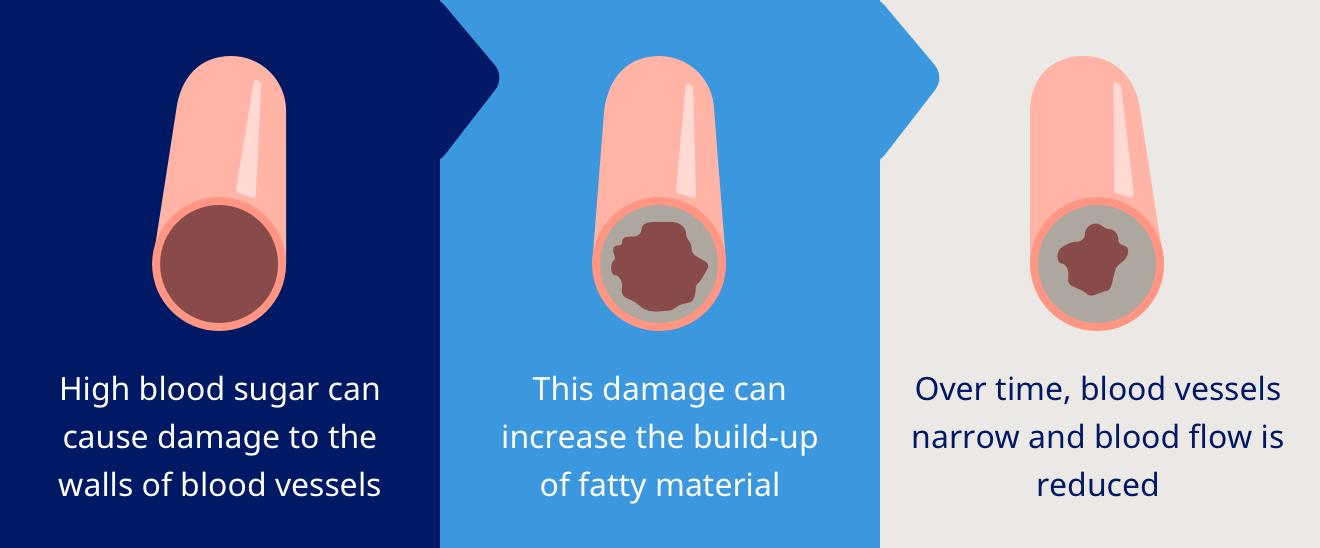
Cardiovascular disease describes a range of disorders that affect the heart and circulatory disease, usually due to atherosclerosis (a build-up of fatty deposits inside the arteries) or hypertension (high blood pressure). These conditions can lead to restricted blood flow and increase the risk of serious events like heart attacks or strokes.
The most common forms include:
Atherosclerosis plays a central role in many cardiovascular conditions. In people with type 2 diabetes, high blood sugar levels promote the buildup of plaque in arterial walls, making them more prone to rupture and clot formation. This accelerates the development of atherosclerotic cardiovascular disease (ASCVD) and ischemic heart disease, increasing the risk of heart attacks, strokes, and further cardiovascular disease3.
People with diabetes are nearly twice as likely to have heart disease or stroke compared to those without diabetes4. Furthermore, hypertensive and atherosclerotic cardiovascular disease is especially common in people with both high blood pressure and poor glycaemic control, contributing to their increased risk of further health complications.
In clinical practice, cardiovascular disease is often classified using ICD-10 codes for accurate diagnosis and billing. For example:
These classifications help tailor treatment plans and track outcomes over time.
Symptoms of cardiovascular disease can vary depending on the condition, but many share overlapping features, and some are exacerbated by physical inactivity. Early signs are often subtle or mistaken for other conditions, especially in people with diabetes, where nerve damage may dull pain perception.
People living with hypertensive cardiovascular disease or arteriosclerotic cardiovascular disease may not experience noticeable symptoms until a major event, such as sudden cardiac arrest, a heart attack, or stroke, occurs.
Because symptoms can be mild or develop gradually, regular check-ups are crucial - particularly for individuals with diabetes5. Tests such as ECGs, cholesterol panels, blood pressure readings, and imaging (e.g., echocardiograms or coronary calcium scans) can help identify issues before complications arise.
Receiving a diagnosis of cardiovascular disease can feel daunting, but it doesn't mean the end of a full and active life. Just like those living with diabetes, many people live well with cardiovascular disease through a combination of treatment, lifestyle changes, and ongoing monitoring.
Managing cardiovascular disease involves a multi-faceted approach:
You don’t have to manage cardiovascular disease alone. A strong support team may include:
It’s common to feel overwhelmed or anxious after a diagnosis. Cardiac rehabilitation programmes, peer support groups, and therapy can help people rebuild both physical stamina and emotional wellbeing8
Whether you're managing type 2 diabetes, have a family history of heart disease, or simply want to protect your long-term health, there are clear steps you can take to reduce your cardiovascular risk.
Small, sustainable changes in behaviour can lead to significant health benefits.
For individuals with moderate to high cardiovascular risk, lifestyle changes alone may not be enough. Medications can help manage:
Your doctor will assess your individual cardiovascular disease risk factors and determine whether medication is appropriate for prevention or treatment.
Navigating a new diagnosis can be confusing. One of the most important things you can do is to ask questions and stay informed.
Engaging in shared decision-making improves cardiovascular health outcomes and empowers you to be an advocate for your care10.
Cardiovascular disease is a serious condition - especially when combined with type 2 diabetes, but it is treatable and often preventable. By adopting a heart-healthy lifestyle and addressing potentially modifiable risk factors, following medical advice, and staying engaged with your healthcare team, you can significantly reduce your risk and live a longer, healthier life.
Whether you're newly diagnosed or simply concerned about your risk, the best time to act is now. Through awareness, early detection, and personalised care, you have the power to protect your heart health.
Start by talking to your doctor to understand your condition and treatment plan. Follow their advice closely regarding blood pressure levels and ask questions if anything is unclear.
You should also adopt a heart-healthy lifestyle: avoid an unhealthy diet, eat well, exercise regularly, quit smoking, limit alcohol, and manage stress.
Take your prescribed medications as directed and keep up with follow-up appointments to monitor your progress. With proper care, many people manage cardiovascular disease and live active, fulfilling lives.
Cardiovascular disease usually can’t be fully cured, but it can be effectively managed. With lifestyle changes, medications, and medical care, many people control their symptoms and reduce the risk of complications. Early detection and consistent cardiovascular disease treatment can help prevent the condition from worsening and allow individuals to lead healthy, active lives.
Yes, many people around the world are living with cardiovascular disease. It’s one of the most common health conditions globally. Many individuals manage it successfully with lifestyle changes, treatment, and support. You're not alone - connecting with support groups or others facing similar challenges can provide encouragement, guidance, and a sense of community.
HQ25DI00139
