“I don't use the word diet. It's a meal plan.”
Eating healthy is important for everyone, but it's even more important for people living with type 2 diabetes. A healthy, balanced diet is – together with exercise – your most powerful tool for managing the disease.
From childhood to old age, food is central to social life. Meals structure the day and define relationships with other people. Furthermore, what gets served and eaten depends on occasion, time of year, cultural norms and more.
To help you navigate through all that, I have put together some tips and pointers which will make living and eating with diabetes both enjoyable and easy.
If you're newly diagnosed with diabetes, you might be wondering what it will mean for the way you eat. You may worry that you don't know enough about diet and nutrition to establish the food habits that work and keep symptoms manageable.
“I don't use the word diet. It's a meal plan.”
Let’s get into it! First, try not to think of yourself as someone “following a diet”. Why not say “meal plan” instead? It’s not set in stone, after all! You could always revise it if something doesn’t work out for you.
The plate method
Carb counting
The Glycaemic Index method
The easiest of the three, this method reminds you that no single food group provides you with all the energy and nutrients you need.
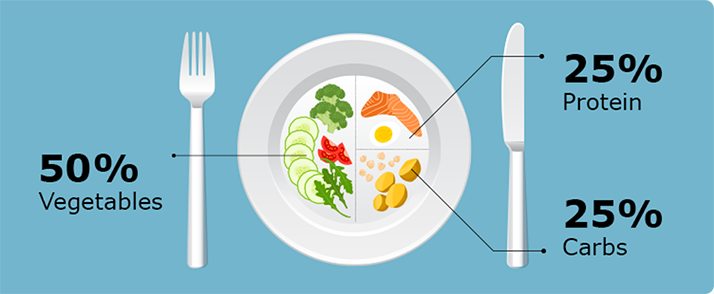
Many people living with type 2 diabetes can control their blood sugar levels by simply getting portion sizes right. Instead of counting carbs – which we’ll get to in the next method – the plate method offers a quick visual shortcut to healthy balanced eating.
Learn it, apply it to three meals per day, and you won’t go entirely wrong.
Why is it called the plate method? Because it requires you to look at your actual plate (9 inches across is the ideal size). Now divide it into 4 quadrants. As you put food on the plate, cover 2 quadrants with non-starchy vegetables (such as broccoli, spinach or cabbage), 1 with lean protein (such as white-fleshed fish or white-meat poultry without the skin) and 1 with carbohydrates (or carbs). Carbs include grains, bread or starchy foods but are found in other foods as well.
Whether you also need snacks in between meals depends on your insulin regimen. Your doctor, nurse or dietitian can give you further advice on adjusting your carb intake with your insulin dose.
Do people living with diabetes need to avoid carbs altogether? No! In fact, that would be a mistake because carbs coexist with important vitamins and minerals in many foods.
“When I’m carb counting, I’m not depriving myself of any carbs. I’m exchanging the carbs.”
When it comes to carbs, you need to learn to count them. That lets you do two things: keep your blood sugar level under steady control and provide your brain and muscles with the fuel they need to function.
Successfully managing diabetes is all about discovering how what you eat and enjoy – and also when you eat – affects your blood sugar levels and your overall health, including your mood. Specifically, here we’re talking about carbs.
Living with diabetes is all about controlling the glucose level in the blood. And because carbs are turned into glucose when absorbed, people with diabetes need to be mindful of their carb intake.
Women with diabetes typically aim for 45-60 grams of carbs per meal (60-75 for men) – and a third of that per snack. What matters when you count carbs is the amount – not the type. That’s where food labels come in.
Find the "Total Carbohydrate" number on the "Nutrition Facts" panel of the food (if packaged). This will tell you how many grams of carbs you use up out of your total carb average per meal by eating one serving size.
Do the same for other foods you plan to eat. Aim for your carb window – not by depriving yourself of foods you like, but by eating them in moderation. Make your meal plan diverse and exciting!
Fresh foods without a label force you to guess the number of carbs they contain. A good rule of thumb is that a serving of fruit, milk or starch has about 15 grams of carbs. Get yourself a pocket guide or app that lists carb counts and portion sizes.
The precise amount of grams of carbs you need depends on how physically active you are and which medicines you take. Your doctor or a registered dietitian can help you identify the right balance.
Here’s something you need to know about carbs: They come in a simple and complex type. If you are living with diabetes, complex carbs are better for you because they take longer for your body to digest and absorb, which means that they act as a buffer against fluctuations in blood sugar level – also known as hypoglycaemia and hyperglycaemia.
So aim to get the majority of your carbs from nutrient-rich and slow-acting complex carbs. Choose brown rice, oatmeal, quinoa, farro, millet and bulgur over simple carbs such as processed and refined sugars. And go “whole-meal” if possible when you choose breads, pasta and crackers. A great tip for eating out or travelling is to download an app that gives you a quick overview of food types that are unfamiliar to you.
You now know that the amount of complex and simple carbs in a given food is relevant to how much you can eat. But there’s another method you need to know: the glycaemic index.
The glycaemic index ranks food on a scale of 0 to 100 according to the food’s impact on your blood sugar. The higher the index, the quicker the food is digested and absorbed, leading to an increase in the level of glucose in the blood.
Maybe you are particularly fond of certain foods. If that’s the case, I suggest looking up their glycaemic index first. You need to know how they score in terms of quickly causing your blood sugar levels to rise, because your safety, well-being and ability to function depend on this. As you get used to this method, you’ll gain a sense of how much – or how many – of a certain food type you can eat without causing your blood sugar levels to either plummet or spike.
Many people living with diabetes find that there are certain foods they have to cut out – completely. But you can choose a “glass half-full” way of looking at groceries. Give a little thought to your grocery shopping and you won’t run out of interesting options in the kitchen.
“There are these things that are on my I Don't Eat That Anymore list.”
A great tip when you go to the supermarket is to spend more time among the fresh produce than the packaged foods. You can generally find the healthiest foods along the perimeter of the store. Don’t rush past them in pursuit of processed foods, and try to concentrate on fruits and vegetables as well as dairy, meat, chicken and fish.
Why this prioritisation? Because the dietary pitfalls primarily haunt packaged and canned foods. If you read the food label this fact will be clear as day. (Always consult the food label so you avoid surprising reactions to the food.) And needless to say, some packaged foods are perfectly fine for someone living with diabetes – e.g. canned tuna, beans and oatmeal.
Here’s another tip that is both easy and charming. When you go grocery shopping and consider buying a new type of food, ask yourself if your great-grandmother would have recognised it. If the answer is yes, then you probably don’t have to be suspicious of its nutritional value.
Another really useful tip touches on the colour of foods. Darker foods are to be preferred over lighter variants. Pick spinach over iceberg lettuce, brown rice over white rice, sweet potatoes over white potatoes, etc. Skip pale foods and opt for whole-grain ones as they will balance your blood sugar and raise your general well-being.
When you go out to a restaurant, the trick is to keep your focus! Don’t let the many options throw you off your “meal-plan” game.
Consider and plan your way through the whole meal – from a starter through the main course to dessert. Focus on the carbs in each dish and use an app to help you do the estimates (unless the menu provides the nutritional details).
“I always view dessert as: it's my entire carb count for the meal.”
So what about dessert? Some people with diabetes use the rule of thumb that having dessert uses up all the carbs they can have for the meal. So choosing dessert means having a salad instead of a carb-heavy starter and main course. This is why it’s important to consider your entire meal from start to finish, before you make any final selections.
When there is a buffet, the same advice applies. Familiarise yourself with all the options before you dig in, otherwise you’ll likely run out of carbs before you make it to some of the foods you were looking forward to.
Living well with diabetes will make you a pro at putting together a delicious meal without breaking the rules on which your well-being hinges.
People who love to push food on you are a special kind of challenge for people living with diabetes. They may say things like “Just take a little piece” or “I made it just for you” or “My feelings will be hurt if you don’t try this.” Typically charming and well-meaning, they unfortunately make sticking to a meal plan a bit more difficult. Occasionally, food pushers constitute a real problem.
Food is about more than metabolism. It is a big part of daily socializing, and is tied to relationships, love and warmth – often with people we don’t want to reject. Having to reject the food they try to offer can feel like rejecting their love or otherwise putting a damper on the relationship.
There may be no easy way out when a food pusher threatens to upset your meal plan, but here is a tip anyway. Smile and say, “I can’t eat that now but I’ll save it for later.”
Living with diabetes means putting your health and well-being before other concerns and priorities. This is not selfishness. It is a prerequisite for being useful and available to those who matter to us.
Living with diabetes is a journey, and you’re always moving forward. Some days will be better than others. Some days your methods and metabolic rhythm are going to be a perfect match – and some days you’ll wonder what you’re doing wrong.
“Sometimes I get the diabetes management right. And then there are days where I’m like, It just didn’t pan out perfectly today.”
When you get it wrong, the first rule is: Don’t beat yourself up! A day that didn’t pan out perfectly is not the end of the world – and you shouldn’t carry the disappointment forward with you. If something goes wrong at breakfast, you can still ace lunch! If the balance is off at lunch, you can still succeed at dinner! And if a whole day leaves you unimpressed with yourself, look ahead to tomorrow and aim to do better.
A person with diabetes has essentially the same nutritional needs as someone without the condition. This means that no special foods are necessary for those with diabetes. As with any healthy eating program, those with diabetes should focus more on their overall dietary pattern than obsess over specific foods.
However, people living with diabetes have a good reason to avoid some of the things that can more freely be enjoyed by those without diabetes. As we have seen, the role of carbs is central to building a meal plan when living with diabetes. This is a clue to the differences between how people with and without the condition can approach their food intake. Take simple carbs such as are found in candy, cakes, soft drinks, white bread and white rice. These can be useful when your blood sugar level runs low, but are not conducive to stable blood sugar levels for someone living with diabetes.
The glycaemic index will suggest which foods someone with diabetes might try to limit or avoid – and the reverse. High-fiber, slow-release carbs should be favoured over foods that merely spike your blood sugar level. For instance, high-fiber, low-sugar cereal is to be preferred over a sugary breakfast cereal. Peas or leafy greens are to be preferred over corn, and so on.
A type 2 diabetes diagnosis doesn’t mean you can no longer enjoy food. Committing to a healthy and realistic meal plan means that food can still be a delightful and satisfying part of your life. If you adopt a mindset that respects the needs of your body, you can live life to the fullest. When you review some of your habits around food, you’ll find that living with diabetes can actually reveal many exciting options. There are countless new foods and recipes waiting to be discovered!
This is general disease awareness and should not be understood as medical advice. If you have any questions or concerns, you should contact your healthcare professional.