
MANAGE YOUR DIABETES WITH EXERCISE
A healthy diet and increased exercise are usually the first things you are encouraged to try in the early stages of type 2 diabetes.
Meet Eva who struggles getting her diabetes numbers right
For those with type 2 diabetes, learning how to keep glucose within a safe range can prevent serious health problems and improve long-term wellbeing. With consistent monitoring, healthy lifestyle changes, and the right treatment plan, including working closely with your care team, it’s possible to reduce the risk of complications and maintain better control over your diabetes condition2.
Type 2 diabetes affects the way your body processes glucose. This can result in high blood sugar, also known as hyperglycaemia, which can damage various organs over time if left untreated3. The goal of diabetes management is to maintain normal blood sugar levels within a safe and steady range.
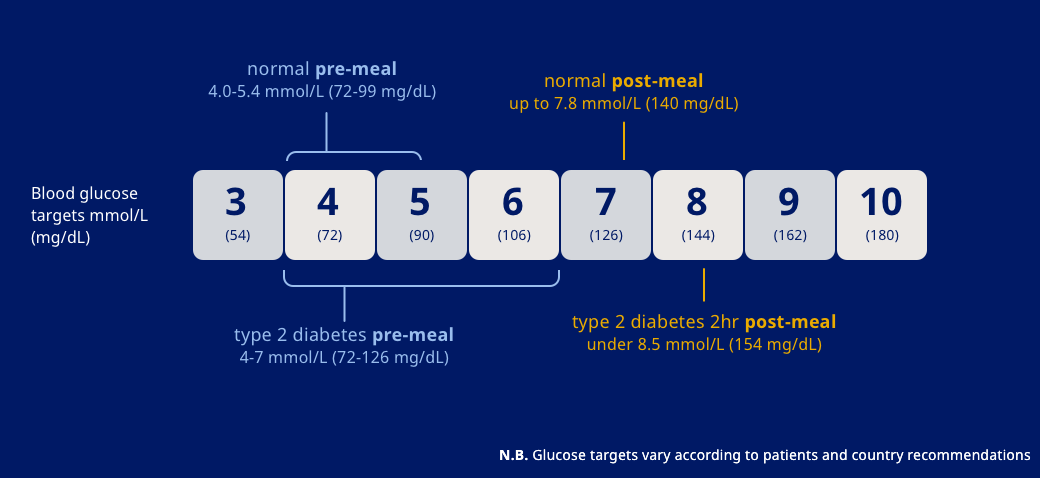
For most adults living with diabetes, the recommended blood sugar level targets are:
These are general targets and may vary based on age, overall health, diabetes duration, and diabetes medicine treatment type. For example, some older adults or individuals with other health conditions may benefit from slightly higher targets to reduce the risk of hypoglycaemia, as advised by a doctor or healthcare professional.
Understanding what level of blood sugar is dangerous for type 2 diabetes, often determined through a blood test to diagnose diabetes, is key to taking early action4. Levels above 240 mg/dL (13.3 mmol/L) are considered high, and anything over 300 mg/dL (16.7 mmol/L) could be dangerous and lead to serious complications - particularly if symptoms are present or levels remain elevated over time.
Very high blood glucose (e.g. over 600 mg/dL or 33.3 mmol/L) may signal a life-threatening complication related to developing diabetes like hyperosmolar hyperglycaemic state (HHS), especially in people with type 2 diabetes5. Signs to be aware of include:
If these symptoms appear alongside a very high reading, seek urgent medical attention.
Regularly checking your blood sugar gives you essential insights into how food, medication, stress, and physical activity affect your glucose levels6. This empowers you to make timely decisions and tailor your care plan, accordingly, including the importance of exercising regularly.
Blood glucose meters are small devices that give you a snapshot of your current blood sugar level using a finger prick test7.
How to use a glucose meter:
Your doctor will advise how often you should check your blood sugar, but typical times include:
A CGM uses a sensor placed just under the skin, usually on the abdomen or upper arm, to continuously measure glucose levels, especially if there is a family history of diabetes. The device sends data to a reader or smartphone app7.
Benefits of a CGM:
CGMs are especially helpful for people on intensive insulin therapy or those with frequent fluctuations in their blood sugar levels due to their diabetes medications7.
Recording your results - manually or via an app - helps identify trends and triggers that influence your glucose control. Take care to note following:
Sharing this data with your doctor and/or healthcare team helps support more personalised decisions around your treatment for diabetes7.
Hyperglycaemia is dangerous both in the short and long term, especially when coupled with stress and/or high blood pressure8. Left unmanaged, high blood sugar can lead to severe medical emergencies or cause gradual damage to vital organs, including affecting red blood cells.
Hyperglycaemia can occur for various reasons, including:
Recognising what causes your blood sugar to rise can help you make better choices and take early action.
Though more common in type 1 diabetes, DKA can also occur in people with type 2 diabetes. It happens when the body uses fat for fuel due to a lack of insulin, leading to a build-up of acids called ketones10.
Symptoms of DKA include:
DKA is a medical emergency and requires immediate treatment.
HHS is a complication primarily associated with type 2 diabetes and various risk factors that can exacerbate the condition5. It’s marked by dangerously high blood glucose levels and severe dehydration, often triggered by illness or missed medication.
Symptoms include:
Like DKA, HHS is life-threatening and needs urgent medical intervention.
Prolonged high blood sugar levels damage the blood vessels and nerves, leading to multiple complications.
People with diabetes are at significantly higher risk of heart disease and stroke, making losing weight an important goal for reducing this risk11. Hyperglycaemia contributes to the narrowing and hardening of arteries (atherosclerosis), which can lead to cardiovascular events.
High glucose damages the tiny filters in the kidneys, especially when combined with certain medicines, if the body does not produce enough insulin - eventually leading to kidney failure if not managed properly11.
Symptoms include:
Regular kidney function tests are essential.
Diabetes can damage the small blood vessels in the eyes, leading to symptoms such as:
These complications may cause vision loss if not detected early. Annual eye exams are strongly recommended.
Diabetic neuropathy affects about half of all people with diabetes13. It typically begins in the feet or legs and can cause:
Nerve damage increases the risk of foot injuries, infections, and even amputations13.
Chronically high blood sugar impairs circulation and immune function, making it harder for the body to heal cuts and bruises, highlighting the importance of an exercise programme and regular blood sugar tests14. Even minor injuries can become infected if left untreated.
While medication is important, including knowing how to use insulin properly, lifestyle choices are the foundation of good blood sugar control2. Daily habits make a significant difference in your ability to maintain target glucose levels and prevent complications.
Choose foods that are:
Avoid sugary drinks and snacks. Using smaller plates, measuring portions, and spacing meals evenly can help avoid spikes in blood sugar2.
Exercise increases insulin sensitivity, helping the body use glucose more effectively14 .
Recommended activity:
Even small changes, like taking the stairs or walking after meals, can be beneficial.
Whether you're using a glucose meter or engaging in continuous glucose monitoring (CGM), tracking your levels helps you understand how your body responds to different inputs, which may mean needing more insulin7.
Never skip or alter doses without consulting your healthcare provider or discussing other medicines you may be taking, as this can lead to low blood sugar. Some people with type 2 diabetes will eventually require insulin - this is a normal part of disease progression, not a failure.
Stress hormones can increase blood sugar. Managing stress through meditation, breathing exercises, light movement, or speaking to a friend can make a measurable difference in your levels, especially for those at risk of gestational diabetes8,15.
Sticking to a routine helps stabilise your blood sugar. Aim for regular sleep, meal timing, exercise, and medication. Consistency creates predictability in how your body processes glucose14.
The best times to check your blood sugar depend on your treatment plan and type of diabetes to maintain levels within a healthy range. Common times include before meals, 1-2 hours after eating, before bed, and before or after physical activity, especially when combined with healthy foods. If you take insulin or experience frequent highs or lows, more frequent testing may be needed. Always follow your doctor’s guidance.
Blood sugar levels are generally considered too high (hyperglycaemia) when they are above 130 mg/dL (7.2 mmol/L) before a meal or above 180 mg/dL (10 mmol/L) two hours after eating. However, target ranges can vary based on your age, health condition, and treatment plan. Always follow the target range recommended by your doctor.
People with type 2 diabetes can have small amounts of sugar, but it should be limited and balanced within a healthy diet that supports weight loss . Focus on natural sugars from fruits and avoid added sugars in sweets, sugary drinks, and processed foods. Instead, prioritise whole grains, lean proteins, and fiber-rich foods. Always follow your doctor’s advice for personalised guidance.
HQ25DI00141
